Neuroinflammation
By Professor Pieter Fourie, 2025
Immunoglobulins
Following international observations there is a rapid increase in the incidence of children on the autistic spectrum (ASD) in South Africa. Likewise, children with PANDAS (paediatric autoimmune neuropsychiatric disorder associated with A Streptococcal infection) are also on the rise. Personal observations of both these neuropathologies have been met with an upsurge that is both disturbing and challenging.
A large amount of research has gone into understanding the neurobiology of both entities. Clearly, an underlying autoimmune derangement is at play here. It has been demonstrated that in some children with autism, an abnormal gut microbiome played a role in triggering an autoimmune response. There again, in PANDAS, the basic underlying inflammatory processes causing the derangement of the basal ganglia are the result of antibodies directed against the latter.
Thus, the question arises whether a cross-link exists between the two pathologies. Initial results indicated that around 17% of children with ASD could have underlying PANDAS. Again, it seems that this co-arrangement is on the uprise.
Management for both pathologies are very similar with the aim being addressing the target symptom domains i.e. concentration, irritability, OCD, ticks, mood disorders, and anxiety. Psychological interventions seem to be limited whereas there is a move towards pharmacological support. IVIG has recently been demonstrated to have a dramatic effect in PANDAS where in ASD it has not been so effective. One reason may have been the timing of the intervention as with ASD the neural apoptosis has already taken place by the time IVIG was instituted. The rationale behind the administration of IVIG is based on the effect it has on the neuro-inflammation that exists in children with either entities.
In the developing world, the exorbitant cost of IVIG excludes most patients from the benefit. Recently a program administering intramuscular immunoglobulins (Intragam) for PANDAS has demonstrated a surprising advantage in curtailing the severity of ticks. Although anecdotal, it opens up a cost-effective opportunity to administer pooled immunoglobulins to a wider population. At the same time, it might also lead to the administration of immunoglobulins as an early intervention for children with profound ASD.
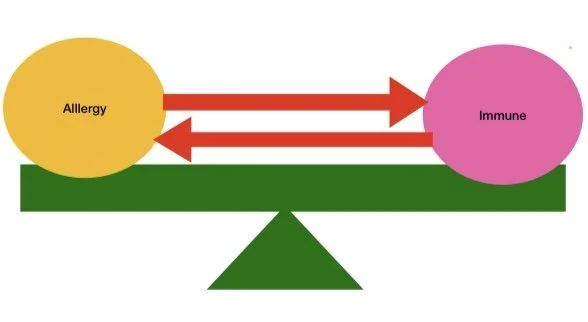
The balance between allergy related symptoms, the immune system, and auto-immune diseases has extensively been discussed in numerous research publications. The hygiene theory, supported by an equal amount of information, indicate that there has been a shift away from a Th1 (attacking bacteria) to a Th2 (responding to allergens) response potentially caused by the industrialisation, overuse of antibiotics, and our under exposure to unrefined nutrients and soil bacteria.
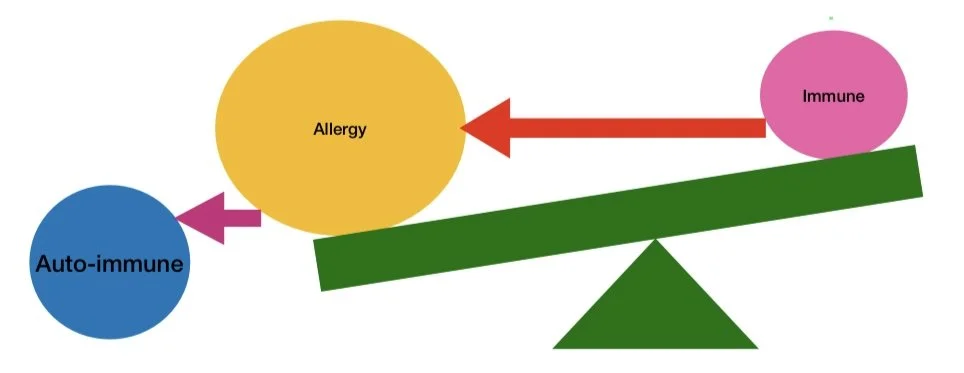
This is backed up by changes in the gut commensal of infants born via the caesarian route. The balance between the immune system and sensitivity to allergies depends on the exposure to specific allergens. The more allergic, the more the balance moves towards an “allergic overweight”. Finally the system moves so far towards an allergic overweight that the immune system becomes deranged and starts “attacking” the body, the so called auto immune reaction.
The recent increase in auto-immune diseases has been characterised by a parallel increase in the neurodiverse population with autism leading the pack and paediatric acute onset neuropsychiatric syndrome following suite. Although a direct causal relationship is difficult to establish, research has demonstrated the presence of neuro-inflammation as a result of an increase in the Th2 response. In layman’s terms it means that our body has moved from a defensive mode to a reactive mode attacking outside invaders (allergens) and in extreme cases turning onto our own cell surface antigens (auto-immune). Behavioural changes should be instituted as early as possible including more natural and home births, often playing outside thereby increasing exposure to soil bacteria, and increase in uncooked nutrients such as vegetables and fruit. Optimisation of the iron levels, the vitamin D status, and adequate intake of essential B vitamins such as folic acid and cyanocobalamin should be included in the realignment of our immune system.
In the case where a change in the allergy status (IgE increase) and/or decrease in the immune system response (decrease in IgA and IgG) can be demonstrated, the challenge will be to decrease exposure to the offending allergens (dietary and environmental avoidance) and an improvement in the immune response through natural interventions such as echinacea. If this proves to be unsuccessful, then pharmacological agents such as antihistamines, leukotrine receptor blockers, and in serious cases pooled immunoglobulins should be considered and administered.
Obviously it becomes a challenge once the neuro-inflammation has already led to structural neural changes and apoptosis. Fortunately the brain demonstrates neuroplasticity up to the third decade, aiding in combatting the neural onslaught. Therapeutic modalities such as neuro-feedback have demonstrated some benefit whereas pharmacological agents e.g. sodium valproate, selective serotonin re-uptake inhibitors, and prefrontal cortex stimulants have clear benefits in improving neural conductivity. The future star wars will be aimed at our own immune system and hopefully we will see a return to a more natural and healthy way of living. In the meantime, we will have to make use of all the means we have at our disposal including the drug armamentarium such as used in autism and PANDAS.